FOLLOW-UP AFTER COLONOSCOPY AND REMOVAL OF POLYP
After the colonoscopy, the endoscopist will provide follow-up recommendations to patients and referring physicians. Recommendations for follow-up after normal colonoscopy among individuals age-eligible for screening and after polyp removal in all individuals with polyps are among the most clinical situations requiring guidance.
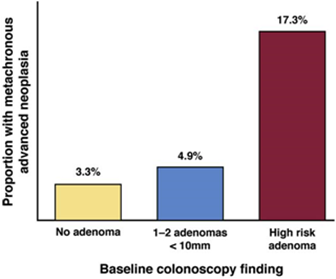
In addition, the risk of metachronous advanced neoplasia is associated with findings on the previous colonoscopy that require special attention. The risk for metachronous adenoma among individuals with no adenoma was 3.3%, 4.9% when 1-2 adenomas <10mm were removed, 17.3% at advanced adenomas had previously been removed.
After a high-quality colonoscopy (see colonoscopy), patients who are not found to have any neoplasia are at the lowest risk. Those with polyps are risk-stratified based on the histology, number, location, and size of polyps detected.
These recommendations do not apply to individuals with hereditary CRC syndrome (e.g., Lynch syndrome and familial adenomatous polyposis), inflammatory bowel disease, personal or family history of CRC (including malignant polyps), or serrated polyposis syndrome.
Terminology, definition
Average risk of colorectal cancer: individuals with no personal history of inflammatory bowel disease, a personal or family history of colorectal cancer, hereditary syndrome associated increased risk, serrated polyposis syndrome.
Normal colonoscopy: endoscopy with no adenoma, sessile serrated adenoma/polyp or sessile serrated polyp (SSP: sessile serrated polyp), hyperplastic polyp (HP: hyperplastic polyp) 10 mm, traditional serrated adenoma (TSA), or colorectal cancer (CRC: colorectal cancer). Individuals with only HP <10 mm were considered to be a normal colonoscopy (no tumor).
Low-risk adenoma: 1–2 tubular adenomas present with low-grade dysplasia (no progression), each <10 mm in size.
There are 2 types of higher risk: advanced adenoma and advanced neoplasia.
Advanced adenoma: when 1 or more of the following features are present:
Adenoma ≥ 10mm in size
Adenoma with tubulovillious/villious histology
Adenoma with high-grade dysplasia
Advanced neoplasia: when 1 or more of the following features are present:
Adenoma ≥ 10mm in size
Adenoma with tubulovillious/villious histology
Adenoma with high-grade dysplasia
Colorectal cancer
High-risk adenoma: when 1 or more of the following features are present:
Advanced neoplasia
≥ 3 adenomas
RECOMMENDED FOR POST-COLONOSCOPY FOLLOW-UP IN AVERAGE-RISK ADULTS WITH NORMAL COLONOSCOPY OR ADENOMAS
|
Recommended interval for surveillance colonoscopy |
Baseline colonoscopy finding |
|
10 years |
. Normal colonoscopy . ≤ 20 hyperplastic polyps, < 10mm |
|
7-10 years |
. 1-2 adenomas, < 10mm |
|
5-10 years |
. 1-2 sessile serrated polyps < 10mm |
|
3-5 years |
. 3-4 adenomas, < 10mm . 3-4 sessile serrated polyps, < 10mm . Hyperplastic polyps ≥ 10mm |
|
3 năm years |
. 5-10 adenomas . 5-10 polyp sessile serrated polyps . Adenoma or sessile serrated polyps ≥ 10mm . Adenoma with villous or tubolovillous histology and/or high-grade dysplasia . Sessile serrated polyps with dysplasia . Traditional sessile serrated adenoma |
|
1 year |
. > 10 adenomas |
|
6 months |
. Piecemeal resection of sessile serrated polyp or adenoma ≥ 20mm |
Early follow-up and detection are very important to treat tumors as soon as possible, most effectively, with the least invasiveness, and to ensure the best quality of life for patients. So, not only doctors but patients need to understand to know the monitoring route for themselves.
March 23, 2021
HUNG M. DO, MD, Ph.D
source: recommendations-for-follow-up-after-colonoscopy-and-polypectomy-a-consensus-update-by-the-us-multi-society-task-force-on-colorectal-cancer-2020-march-gie
