TYPES OF COLORECTAL POLYPS AND CANCER RISKS
A polyp is a small growth of excess tissue that often grows on the lining of the large intestine, also known as the colon. Colon and rectal polyps occur in about 25 percent of men and women ages 50 and older. Not all polyps will turn into cancer, and it may take many years for a polyp to become cancerous.
Types of Polyp Shapes
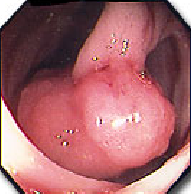
Polyps grow in two different shapes: sessile, flat, and with a stalk (pedunculated).
Sessile polyps are more common than previously thought and harder to detect in colon cancer screening. Sessile polyps do not have a stalk and are attached to the lining by a broad base.
Flat polyps are the least common type of colon polyp and are flat or even slightly depressed. These may be difficult to identify because they are not as prominent as polypoid or sessile polyps, with the commonly available methods of diagnosing polyps.
Pedunculated (Polypoid) polyps look like a mushroom but flop around inside the intestine because they are attached to the lining of the colon by a long, thin stalk.
The types of colon and rectal polyps
The large majority of polyps will not become cancers. Certain types of polyps are more likely to turn into cancer. Removal of polyps during a colonoscopy reduces the risk of developing colon cancer in the future.
The most common types of colon and rectal polyps are:
Adenomatous (tubular adenoma)
About 70 percent of all polyps are adenomatous, making it the most common type of colon polyp. When this type of polyp is found, it is tested for cancer.
Only a small percentage actually become cancerous, but nearly all malignant polyps began as adenomatous. Fortunately, the process for these polyps to turn into colon cancer typically takes many years. With regular screening, they can be found and removed before that happens.
It is divided into 3 types: tubular (tubular - can be found in any part of the colon and stalk), villi (villous - mainly in the rectum and non-petiole, with the highest risk of malignancy), and tubular glands - villi (tubulovillous).
Approximately 15 percent of polyps detected in colon cancer screening are villous or tubulovillous adenomas. This type of polyp carries a high risk of turning cancerous. They are commonly sessile, which makes them more difficult to remove. Smaller villous adenoma polyps may be removed during a colonoscopy, while larger polyps of this type may require surgery for complete removal. The risk of malignancy depends on the size (> 2cm) and the villi's composition.
Hyperplastic
A type of serrated polyp, hyperplastic polyps are common, small, and considered extremely low risk for turning cancerous. Typically any hyperplastic polyps found in the colon are removed and tested to ensure they are not cancerous.
Serrated
Depending on their size and location in the colon, serrated polyps may become cancerous. Small, serrated polyps in the lower colon, also known as hyperplastic polyps, are rarely malignant. Larger serrated polyps, which are typically flat (sessile), difficult to detect, and located in the upper colon, are precancerous.

Inflammatory
Inflammatory polyps most often occur in people who have inflammatory bowel disease (IBD). These polyps are also known as pseudopolyps because they are not true polyps but rather develop as a reaction to chronic inflammation in the colon. Inflammatory polyps are benign and generally do not carry the risk of developing colon cancer.
|
|
HOW COMMON |
CANCER RISK |
TREATMENT |
|
INFLAMMATORY |
Typically found in people with inflammatory bowel disease (Crohn’s disease or ulcerative colitis) |
Low; growths generally benign |
Removal during colonoscopy |
|
HYPERPLASTIC |
Usually small and located at the end of the colon and the rectum |
Considered lower risk |
Removal during colonoscopy |
|
ADENOMATOUS (TUBULAR ADENOMA) |
Most common type – about 70 percent of polyps found in the colon |
Most do not develop into cancer, although larger polyps pose a higher threat |
Removal during colonoscopy; regular follow-ups needed to screen for and remove new polyps |
|
VILLIOUS OR TUBULOVILLIOUS |
Make up about 15 percent of polyps |
Most do not develop into cancer, although larger polyps pose a higher threat |
Can be flat or tougher to remove; smaller villous adenoma are removed during colonoscopy; larger polyps may require surgery |
|
SERRATED ADENOMA |
Make up about 10-15 percent of polyps |
Cause 20 to 30 percent colon cancer |
Hard to detect during colonoscopy |
Genetic adenomatous polyp syndromes
The disease is rare in people who inherit genetic mutations that cause colon polyps. If you have one of these genetic mutations, you have a higher risk of developing colorectal cancer. Early screening and detection can help prevent the growth and spread of these cancers.
Polyps can be detected and safely removed during a colonoscopy, preventing them from turning into cancer. Large polyps may require more than one treatment, and in some patients, surgery could be required for complete removal. If you have an increased risk for colon polyps, talk with your doctor about the types and frequency of tests that will be best for you.
March 12, 2021
HUNG M. DO, MD, Ph.D
